Embarking on the journey of managing your A1C test result levels is akin to charting a course towards better health and well-being, especially if you’re living with diabetes or prediabetes. Picture this: you, equipped with knowledge and determination, working hand in hand with your healthcare team to keep your blood sugar under control. Your A1C level, a trusted indicator of your long-term blood glucose management, takes center stage in this endeavor. In this guide, we’ll explore the practical steps and strategies that can help you navigate this path successfully. From personalized A1C goals and regular blood sugar monitoring to the power of a balanced diet, exercise, stress management, and support, we’ll delve into each aspect of achieving and maintaining your target A1C range. Together, we’ll unlock the keys to effective A1C management, empowering you to lead a vibrant and fulfilling life with diabetes. Let’s embark on this journey to better blood sugar control and overall well-being.
What is the A1C Test?
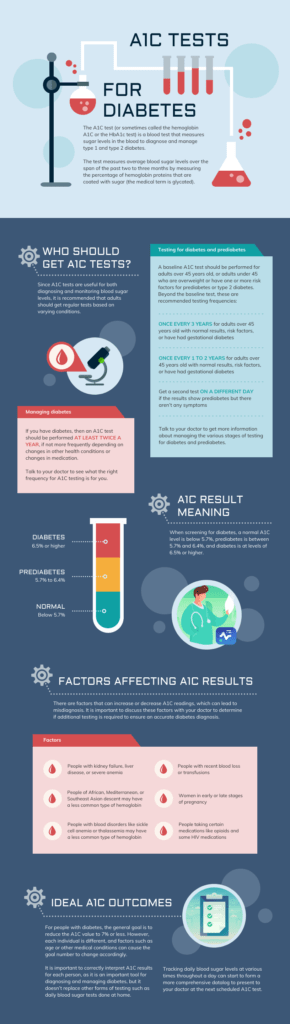
The A1C test, also known as the hemoglobin A1C or glycated hemoglobin test, is a blood test that provides valuable information about a person’s average blood glucose (sugar) levels over the past two to three months. This test is commonly used to monitor and manage diabetes, specifically to assess how well an individual’s blood sugar has been controlled during that time frame.
How Does the A1C Test Work?
The A1C test, also known as the hemoglobin A1C or glycated hemoglobin test, works by measuring the percentage of hemoglobin in your blood that has glucose (sugar) attached to it. Hemoglobin is a protein found in red blood cells, and it is responsible for carrying oxygen from the lungs to various tissues throughout the body.
Here’s how the A1C test works:
- Glucose Binding to Hemoglobin: When glucose circulates in your bloodstream, some of it naturally binds to hemoglobin molecules within your red blood cells. This binding process is directly proportional to the amount of glucose present in your blood at the time. In other words, the more glucose in your bloodstream, the greater the amount that attaches to hemoglobin.
- Red Blood Cell Lifespan: Red blood cells have a lifespan of approximately 120 days, during which they continuously circulate throughout your body. As they travel, some of the glucose molecules attached to hemoglobin remain bound throughout their life cycle.
- Averaging Glucose Levels: The A1C test measures the percentage of hemoglobin that has glucose attached to it, providing an average of blood glucose levels over the past two to three months. Since red blood cells have a lifespan of around 120 days, this test reflects blood sugar control over that extended period.
- Reporting Results: A1C results are typically reported as a percentage. This percentage represents the amount of glycated (glucose-bound) hemoglobin in your total hemoglobin. For example, an A1C result of 7% means that, on average, 7% of your hemoglobin has glucose attached to it over the past two to three months.
Why Is the A1C Test Important?
The A1C test is critically important for several reasons, especially for individuals with diabetes or those at risk of developing diabetes. Here are the key reasons why the A1C test is of significant importance:
1. Long-Term Blood Sugar Monitoring:
The A1C test provides an average of blood glucose (sugar) levels over the past two to three months. Unlike daily glucose checks that offer snapshots of your blood sugar at a single moment, the A1C test offers a broader picture of your overall blood sugar control over an extended period. This long-term monitoring is crucial because it captures trends and variations in your blood sugar management that may not be apparent from daily measurements alone.
2. Treatment Adjustment:
Healthcare providers use A1C results to make informed decisions about the management of diabetes. If your A1C levels are consistently high (indicating poor blood sugar control), it may suggest the need for changes in your treatment plan. Adjustments in medication, diet, exercise, or lifestyle can be recommended to help bring blood sugar levels within the target range.
3. Diagnosis and Risk Assessment:
The A1C test is also used for diagnosing diabetes and assessing the risk of developing the condition. In general, an A1C level of 6.5% or higher is indicative of diabetes, while levels between 5.7% and 6.4% may suggest prediabetes, a condition in which blood sugar levels are elevated but not yet in the diabetic range. Early detection and intervention in prediabetes can help prevent or delay the onset of diabetes.
4. Reducing the Risk of Complications:
Maintaining good blood sugar control, as indicated by a lower A1C level, is associated with a reduced risk of diabetes-related complications. These complications can include heart disease, kidney disease, nerve damage (neuropathy), vision problems, and circulation issues. Regular A1C monitoring helps individuals and healthcare providers track progress in managing and mitigating these risks.
5. Individualized Treatment Goals:
A1C testing allows healthcare providers to set individualized target A1C ranges for each person with diabetes. These targets take into account factors such as age, overall health, and treatment goals. Having personalized A1C goals helps individuals work with their healthcare team to tailor their diabetes management plan to meet specific health objectives.
6. Motivation and Accountability:
For individuals with diabetes, regular A1C testing serves as a motivator to maintain better blood sugar control. Seeing improvements in A1C levels can be a source of encouragement and motivation to adhere to treatment plans, make healthier lifestyle choices, and actively manage diabetes.
The A1C test is a vital tool in diabetes management. It provides valuable insights into blood sugar control over time, guides treatment decisions, helps prevent complications, and empowers individuals to take charge of their health. Regular A1C testing is an essential component of comprehensive diabetes care and plays a pivotal role in improving the quality of life for individuals with diabetes.
Interpreting A1C Results
Interpreting A1C results is crucial for understanding your blood sugar control and managing diabetes effectively. The A1C test provides a percentage that reflects the average blood glucose levels over the past two to three months. Here’s how to interpret A1C results:
1. Normal A1C Levels: Below 5.7%
- What it means: An A1C result below 5.7% is considered normal and indicates good blood sugar control.
- Action: If you have normal A1C levels and no other risk factors, you’re likely not at risk for diabetes. However, it’s still essential to maintain a healthy lifestyle to prevent future issues.
2. Prediabetes A1C Levels: 5.7% to 6.4%
- What it means: A result between 5.7% and 6.4% is indicative of prediabetes, a condition in which blood sugar levels are higher than normal but not yet in the diabetes range.
- Action: Individuals with prediabetes can make lifestyle changes to prevent or delay the onset of diabetes. This includes adopting a healthier diet, increasing physical activity, and managing other risk factors like obesity.
3. Diabetes A1C Levels: 6.5% or Higher
- What it means: An A1C result of 6.5% or higher typically indicates diabetes.
- Action: If you receive an A1C result in this range, it’s essential to work closely with your healthcare provider to manage your diabetes effectively. Treatment may involve medication, diet modifications, exercise, blood sugar monitoring, and other lifestyle changes.
4. Individualized Target A1C Range:
For people with diabetes, healthcare providers often set personalized target A1C ranges based on factors like age, overall health, and treatment goals. Achieving and maintaining your specific target A1C range is essential for diabetes management.
- Well-Controlled Diabetes: An A1C result within or close to your target range indicates well-controlled diabetes. It suggests that your current treatment plan is effective in managing your blood sugar.
- Suboptimal Control: If your A1C result is consistently above your target range, it may signal suboptimal blood sugar control. In such cases, your healthcare provider may adjust your treatment plan, including medication dosages and lifestyle recommendations.
- Hypoglycemia Risk: On the other hand, if your A1C result is consistently below your target range, it may indicate a risk of hypoglycemia (low blood sugar). Your healthcare provider will need to balance your treatment plan to minimize this risk.
It’s important to note that A1C results are not the sole factor in diabetes management. Your healthcare provider will consider other factors, including daily blood sugar monitoring, symptoms, and overall health, when making treatment decisions.
Regular A1C testing, typically every three to six months, is essential for tracking your progress in managing diabetes and adjusting your treatment plan as needed. Effective diabetes management can help reduce the risk of complications and improve your overall quality of life.
Managing Your A1C Levels: Tips for Success
Managing your A1C levels successfully is a key aspect of diabetes care. A well-controlled A1C level reflects good blood sugar management and reduces the risk of diabetes-related complications. Here are some tips to help you achieve and maintain your target A1C range:
1. Work Collaboratively with Your Healthcare Team:
Establish a strong partnership with your healthcare provider, diabetes educator, and any other members of your diabetes care team. Regular check-ups and open communication are essential for effective diabetes management.
2. Set Personalized A1C Goals:
Work with your healthcare provider to set individualized A1C targets based on your age, overall health, and treatment goals. Having personalized goals helps you stay motivated and focused on your blood sugar control.
3. Monitor Your Blood Sugar Regularly:
Frequent blood sugar monitoring provides real-time information about how your daily activities and choices impact your blood sugar levels. Use a glucose meter as recommended by your healthcare provider and keep a log of your readings.
4. Adhere to Your Medication Plan:
If you’re prescribed diabetes medications, take them as directed by your healthcare provider. Consistent medication adherence is crucial for achieving and maintaining good blood sugar control.
5. Adopt a Healthy Diet:
Follow a balanced and diabetes-friendly diet plan. Focus on:
- Carbohydrate Management: Monitor your carbohydrate intake and aim to keep it consistent throughout the day.
- Portion Control: Be mindful of portion sizes to avoid overeating.
- Healthy Food Choices: Include plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats in your diet.
- Limit Sugary and Processed Foods: Reduce or eliminate sugary snacks and beverages, as well as highly processed foods.
6. Regular Physical Activity:
Incorporate regular exercise into your routine. Physical activity can help lower blood sugar levels, improve insulin sensitivity, and contribute to overall well-being. Aim for at least 150 minutes of moderate-intensity aerobic activity per week, as recommended by healthcare providers.
7. Stress Management:
Stress can impact blood sugar levels. Practice stress-reduction techniques such as deep breathing, meditation, yoga, or spending time in nature to help manage stress effectively.
8. Get Adequate Sleep:
Prioritize good sleep hygiene to ensure you’re well-rested. Poor sleep can affect blood sugar control, so aim for 7-9 hours of quality sleep each night.
9. Regular A1C Testing:
Follow your healthcare provider’s recommended schedule for A1C testing. Regular testing helps you and your healthcare team track your progress and make adjustments to your treatment plan as needed.
10. Education and Support:
Stay informed about diabetes management through educational resources, workshops, and support groups. Connecting with others who have diabetes can provide valuable insights and emotional support.
11. Avoid Skipping Meals:
Eating regular, balanced meals and snacks can help stabilize blood sugar levels throughout the day. Skipping meals can lead to spikes and crashes in blood sugar.
12. Limit Alcohol Consumption:
If you choose to consume alcohol, do so in moderation and be mindful of its effects on blood sugar. Alcohol can cause hypoglycemia (low blood sugar) or hyperglycemia (high blood sugar) depending on the circumstances.
Remember that diabetes management is a journey, and there may be times when you face challenges. Don’t hesitate to reach out to your healthcare team for guidance and support. By following these tips and staying committed to your diabetes care plan, you can work towards achieving and maintaining your target A1C levels and enjoy a healthier, more fulfilling life with diabetes.
Addition information
https://www.diabetes.org.uk/guide-to-diabetes/managing-your-diabetes/hba1c
https://www.cdc.gov/diabetes/managing/managing-blood-sugar/a1c.html
https://www.mayoclinic.org/tests-procedures/a1c-test/about/pac-20384643
